SPEAKING IN PROSE & THE REDISCOVERY OF S.13(1) MHA 1983
By Tim Gorvett
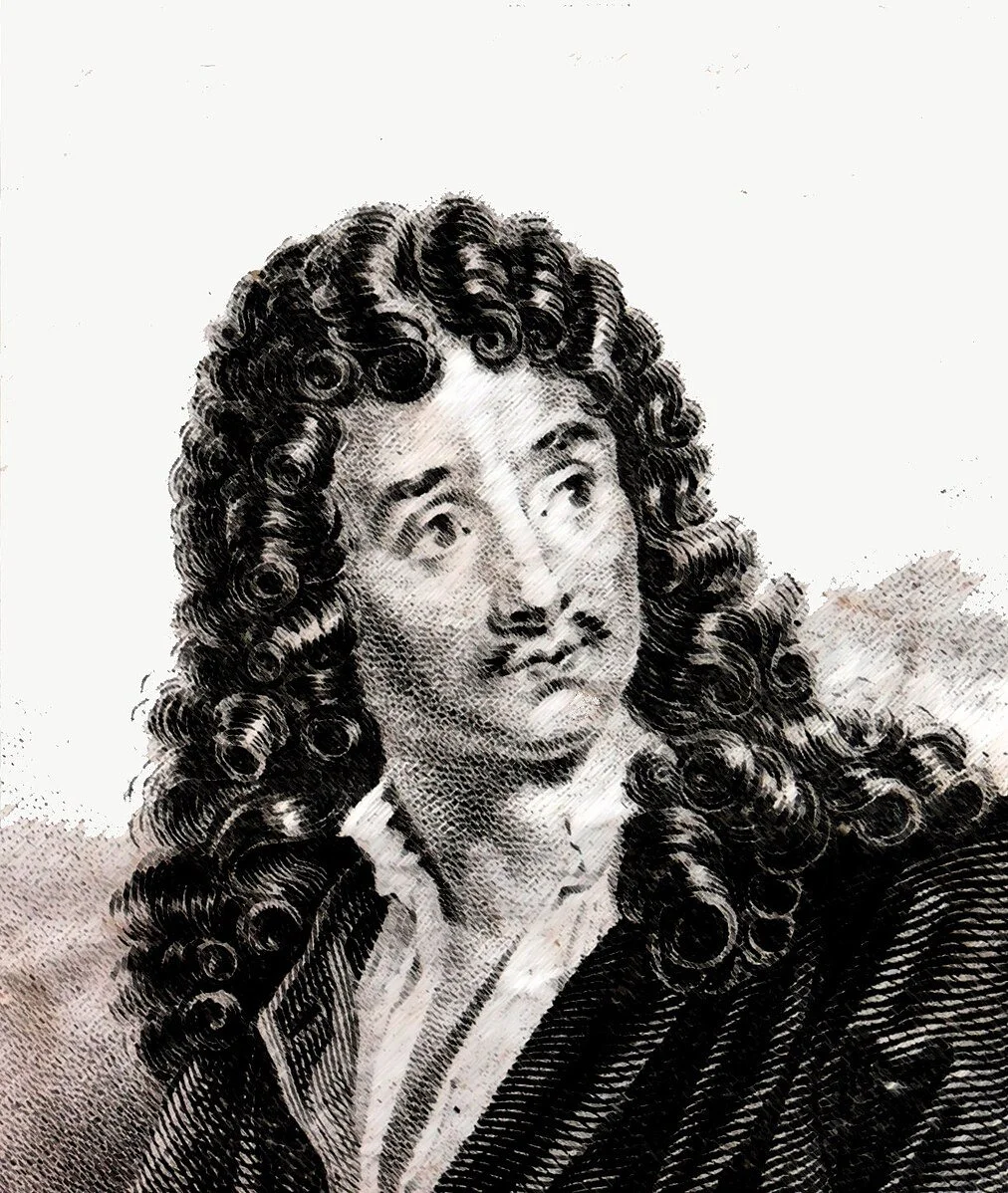
“My faith! For more than forty years I have been speaking prose while knowing nothing of it, and I am the most obliged person in the world to you for telling me so.”
Monsieur Jourdain, ‘Le Bourgeois gentilhomme’ by Molière
John Mitchell and his colleagues have noticed (see the Introduction:4/4 of the 2024 Discussion Paper – reference below) that their recent rediscovery of s.13(1) of the MHA has not met with universal enthusiasm, and they have wondered why this is, laudably calling for wider debate and for critical views to be expressed. Before doing so, it is worthwhile taking a moment to consider why this might be so.
If colleagues are chary of contending in this matter, it may be because the arguments being made so far succeed too well, after all. They are in favour of reducing compulsory admission, of moderating the terrible impact on the global majority population, of taking more quality time on assessments and maximising alternatives to admission, of making our lives as AMHPs easier and more satisfying, and this appears to be the means to these ends. It can come to feel as if to differ is to be arguing against motherhood and apple-pie, against everything that an AMHP stands for. I feel a bit nervous myself.
But it is also because in important ways the proposition itself may be incoherent, and it always difficult to know how to come at such arguments-is it new or is it old, is it self-evident or is it seductively controversial, does it represent a small adjustment in our work, or a grand transformation, will it-crucially-have a large effect or will it like so much tweaking of definitions, turn out quite negligible? Even the language is unstable, bewildering at times-by para.16 we are having to ask, is it even a MHA assessment, or is it really a “MHA assessment”?
As practicing AMHPs, we haven’t got a lot of time, or headspace, or emotional energy, for that matter, to take up an unpopular stance in a debate about ill-defined and rather abstruse points. It is said we have chosen to stay silent, but that’s not quite right, is it?
Anything that stirs us up to think about our work afresh is a good thing, of course. But personally, I think, as to this rediscovery of s.13(1), it may be said to have some new things in it, and some true things in it. The difficulty, according to the old saw, is that the true things are not new, and the new things are not always true.
Let us commence with the idea of consideration, which is extremely important, I agree. The duty under s.13(1) for an AMHP to consider the case is, in fact, the most important duty owed to any individual by a local authority in peacetime, the s.47 child protection duty only apart, and to my mind far and away exceeds the importance of all those Care Act ones, as it touches on the fundamental liberty of the subject, and includes those who have the capacity to make decisions for themselves.
Bu we mustn’t make a fetish of this notion-it is what we do all day, every day.
When I read the paper for the first time, after all, I noted that most of my recent AMHP work had been mere consideration-a s.13(4) case where I twice visited the patient at home with various colleagues offering alternatives to treatment, once in person to the GP surgery (you can never get through on the phone these days), liaised a number of times with the putative nearest relative, with people in her community, with housing officers, and wrote with extensive advice to the proposed patient and her relative before closing the case without an assessment. I had just then put back two other referrals for further work by the home treatment team (one of whom returned to us in a week); in my more senior management role I had been dealing with two instances where consideration of the case by an AMHP had led to action not being taken at a certain time, when perhaps it should have been, an unusual case of denial of pregnancy, and another ending in a death and a high-profile complaint. The position taken by the AMHP incidentally had been of great importance in these last two cases, possibly of excessive importance, as it put off re-referral, pointing up already some of the challenges for the “slow assessment”, which I will touch upon further in a moment.
But in any event, none of this is remarkable, it is what we do all the time as AMHPs.
In the same way, asking AMHPs (para.18) to ponder the implications of attempting an assessment at all, of where and when and how to conduct it, of who should be present, how the make-up of the team influences the outcome, these are questions we have been asking in our approval panels for twenty years, in both the local authorities where I have worked in that time. I would not be satisfied to approve any AMHP who did not attach proper importance to these things, nor is this new either. Are we not in danger of being like Moliere’s M. Jourdain, astonished to learn that we have been speaking prose all our lives?
If anything, the increasing use of warrants for the most intrusive and dramatic of all interventions in pursuit of a consideration of the case, the community assessment in a person’s own home, has interposed a further layer to that consideration, the justification of proposed action not to a local authority manager nor even to an individual AMHP but to a magistrate who may grant or withhold formal authority. The importance of this as a constitutional safeguard and as a practical “hard shoulder” to professional judgement should not be obscured by the fact that, having given a lot of thought to the matter and set out a closely reasoned case, the AMHP’s application is rarely refused. And yet I surmise that the authors are not keen on warrants, and would prefer they were used less, not more.
So what is new about the rediscovery of s.13(1)?
One proposition is that the local authority as such has a role in declining referrals (para.19), before they ever reach the AMHP. But this is decidedly odd. If there is any reason to believe that someone in their area who suffers or may be suffering from mental disorder-a patient, in other words-may need an application to be made, they shall ask an AMHP to consider the case. This is in statute, moreover, not in guidance. I recently dealt with just such an instance, mercifully very rare, where there were shall we say, other priorities for a local authority, than having an AMHP consider the case, they are not pretty. If there is managerial scrutiny this needs to be by an AMHP who is a manager, I shall come back to this later.
More substantial is the argument that there requires to be evidence of the consideration (para.20), and I agree this is also very important, even if most of us, drowning in paperwork, will hear this as a demand for yet another d*****d report, and this time not even of a statutory or Code nature. We are not given anywhere any guidance, as to what such a report might look like, but it will be of a very unique character, being if I understand it, a justification of a decision not to assess, although for consistency’s sake, perhaps it should also be completed in cases where a decision is made to assess, as that decision is now arguably sufficiently problematised and after all, the outcome may still be no detention.
It will be a report, moreover, which does not only have to justify a very strait conclusion, to detain or not to detain, as our reports do now, but which may have to ramble over the whole face of service delivery for the patient, explaining just why this or that may or may not fit the bill: it is (as John Mitchell would agree, I think) a substantial piece of work. It can be difficult to see why such a piece of work would not be better informed, by the AMHP meeting with the patient, and taking into account recommendations made, or not, by qualified medical practitioners, as well as the views of the patient’s relatives.
A third and very prominent feature is certainly new, and that is the constant stress on slowing down the process, and perhaps thereby increasing the chance of it issuing without a MHA assessment at all. From the point of view of using compulsory powers less and of our own working processes, I can’t deny this is one of the most attractive features of the new idea.
I have already suggested above, that significant risk is present in deciding not to carry out a MHA assessment on the basis of the AMHP’s consideration of the case: delay is introduced, relative urgency may be misapprehended, unusual presentations or indicators obvious to those on the spot may be missed, potentially with grave consequences; misunderstandings, complaints, and safeguardings may be generated, there may be legal and professional consequences also; and at the limit, the patient may lose their life, or there may be some other grossly harmful outcome.
I had wanted to advert at this point on some cases, known to me, where these risks had been run, and things have gone badly wrong, not necessarily through any fault of the AMHP, so that we are clear about what happens when AMHPs have displayed that higher level of risk tolerance, built upon their experience and validated by their peers, of which Matt Simpson spoke. It is a measure of the problem that I have not so far found any AMHP who is prepared to give me their blessing to set out a case where this has happened, for the purposes of illustration, so distressing do they find going into the matter again, even after lapse of time and in this extenuated manner.
There are two points at least to make about this, and they both bear on the moral distress and moral hazard of which the s.13(1) paper speaks, indirectly of course, and without straying far or explicitly into the tragic realities of this part of our work.
One is that whilst the AMHP’s decision-making may be thoroughly vindicated by the subsequent enquiry, serious case review or by the coroner in the final verdict, the impact of their having exercised this power of consideration may be frightful for the AMHP concerned. The gravest consequences will have arisen from their decision-making and they may be seen as the chief architect of those consequences. They may not consider that they can continue in the role afterwards, and hand back their warrants. For months, more likely a year or more, their professional, and to a degree personal, life, will be in limbo, dominated by this question: had they considered the case properly? The emotional and personal consequences of having exercised this important power by themselves, even when the correctness of the decision is upheld, will be extreme. Need one hardly imagine how it would be, were the chair of the review, the coroner, or other parties, such as myself as AMHP Lead, to decide not to uphold the decision of the AMHP instead?
The other point is that of course we can strive to mitigate all this, although it is interesting that beyond this lengthy s.13(1) report, it does not seem that the authors of the paper have given much thought to this. The invariable answer to anything that goes wrong in our line of work, of course, the identical outcome of every investigation and enquiry, is: elaborate the process. In my experience all sorts of points of elaboration have been identified at different times, to help with this mitigation of the risks of consideration which the AMHP has run.
They may not have consulted with the AMHP duty manager on the day, for example, and so carried all the responsibility themselves. There almost certainly will have been someone they did not consult with, in a complex case reaching crisis point, and so opened themselves to the charge that something crucial was missed. They will not have had a handy s.13(1) report to show, just case notes and e-mails, no doubt, which the Trust or other parties may be swift to call into question. In our local authority we have had no comprehensive investigation process of our own to demonstrate learning from the case, and on one occasion when we commissioned an independent safeguarding report, not a relevant procedure in my view, it eventually departed so far from the actuality that its author was required practically to disavow it in court.
Now of course we can address these defects, if such they be, by elaborating the process, and we have done; but at the cost of centralising the service, running everything through the duty manager, growing our checklists, attempting to introduce clear documentation points (not I hasten to say, the full s.13(1) report) along the way, and make AMHPs stick to them, being much more attentive to playing the referral game with the Trust community teams, pondering what a proper local authority investigation of cases where things have gone wrong might actually look like, and so inevitably increasing still further the burden of reporting on such occasions. Centralising the decision-making encounters the opposite hazard of giving the AMHP so much support, so many senior people to run the decision by, that we end up fettering their discretion and turning the service into exactly that risk-averse, managerial section-making facility that we all want to avoid.
There are, of course, more important aspects of this problem than how the AMHP ends up feeling about it, more important even than being able to show how robustly we have improved our institutional defences, and I think the reluctance wholeheartedly to embrace the full implications-the new implications, to be precise-of what the authors of the paper believe the rediscovery of s.13(1) to be, also lies in these regions.
Because, again speaking as an AMHP and an AMHP manager, on the rota, on-call for the emergency duty team in Central London, the idea of the slowed-down assessment, the attractive accounts of delicate therapeutic compromises negotiated over a cup of tea in a cosy farmhouse kitchen, seem far removed from the day-to-day experience of such services.
Can I say this?
Did I miss the part where the authors of the paper establish, preferably with data, how doing the “MHA assessment” actually increases the probability of eventual detention? Or is it merely founded on the apparently self-evident point that no actual detention can occur without one? For that is far from the case nowadays, and I am not sure how well across the situation the authors are.
In London for example, there is a document agreed between all the parties involved for the management of amongst other things AMHP case-considerations in the emergency department, the health-based place of safety or the police station, called the Crisis Concordat, which seeks to obtain that consideration, in person, at the location, within four hours of the patient’s arrival there. Only yesterday, it seemed, this was the best practice, to resolve the vulnerable patient’s precarious predicament as quickly as humanly possible, yet now perhaps it is not.
It should be said, that the circumstances within which mental health patients arrive in such a setting as the emergency department of a great London acute general hospital, are shocking. They may arrive at all times of the day or night, after community services have failed to engage or help them either as individuals or as whole demographics, in extremities of mental disorder, very often without any lawful authority to hold them. More or less untrained staff-police officers, security, junior ED nurses, family members-struggle to manage the situation for many hours. All sorts of immediate restraints are applied, by anyone who feels able-I recently arrived at such an assessment to find a screaming patient being held down by six staff, security, RMN’s, health-care assistants, with the nurse in charge waving a hypodermic and saying, in effect, quick, quick, get your assessment done before we have to IM the patient again. And these staff are doing the best they can.
Beds even for the patients in greatest need are no longer even sought until the MHA assessment has been carried out and a trajectory established, and then many more hours, days, even, may pass. Far from being able to pop back and see how the patient is getting on, perhaps reconsider the admission altogether, many AMHPs are simply no longer able to make an application after the passage of time which may elapse before the bed is found, a situation which produces great anxiety in many of us. As the patient is moved around, from police station to ED, from ED to crisis assessment “lounge”, the decision can even drift entirely out of their hands, sometimes with deplorable consequences.
And in the HBPoS’s, the police stations, the endless permutations on crisis-management, mental health assessment suites now so prevalent, similar scenes prevail, with more or less improved degrees of professional intervention but often no better a legal basis for what is happening. Instead our medical colleagues speak of the Grey Zone, into which these patients and their carers pass, or try to blow new life into the cold embers of the doctrine of necessity, as if we were living in the midst of civil war. These patients’ conditions are not being improved by slowing down the process, as Matt Simpson proposed we should do.
I am equally uneasy about the forceful recommendations of the authors when they do turn their attention to these situations, of which they are in part aware. To make out papers directly to the HBPoS, for example, and then demand to know why they cannot admit, is the exact opposite of what I advise AMHPs in my service to do, as there is no proper assurance that they are admitting the patient to a bed, and is likely to prompt some such answer, as that there is no Responsible Clinician willing to take charge of the patient, something which would certainly give me pause when my pen hovered over the pink papers, and I would recommend should give pause to any AMHP.
My thoughts indeed turn in other directions, to s.140 rather than to s.13(1), or to ways of assuring a proper statutory basis for such initial encounters, where extreme outcomes are always more likely. How did we lose the 72-hour holding power for s.136, for example? Why do so many other jurisdictions retain a really short-term holding power, of the order of three days, in hope of resolving acute symptoms and opening the door to shorter admissions, as there is some evidence that they do?
I’m not going to mention resources, because we are all on the same page there, except to say again that whilst true, the implications of the rediscovery of s.13(1) in this respect are not new. We are a dwindling, aging profession, we need more AMHPs, with more energy and ideas, to bring creativity to the consideration of cases; but also more community treatment alternatives, better attuned to the needs of global majority populations, to get in there earlier and in more relevant ways, a real Mental Health Service for all the nation. We need AMHP duty teams, sufficiently staffed, where just as one AMHP has to rush out to the ED to a patient in the most urgent and precarious situation, and with the power to resolve it, another AMHP is painstakingly working through the complex community or ward referral, regrouping the resources around the patient to avoid another militarised home-invasion, another revolving-door admission, another fruitless spell in rehab. When I trained for approval, it was with five other colleagues from the same borough, all posts backfilled, all AMHPs to this day: nowadays we are lucky to send one a year, and carry the cost ourselves. This is all true, it is not new.
The object, as it seems to me, at length, is crucial, and we may have become confused about this along the way, not least by well-meaning political interventions. I’m left still with the same questions: is it self-evident or wildly controversial, is it a big change or a small one, would it have a big effect or just pass unnoticed-is it right to manage high demand for admissions in racialised groups, in particular, whatever the cause, by simply suppressing the level of admissions?
Is it not the case, that our object is not to detain less, because levels of detention are a function of general morbidity and acuity, but to obtain the best outcome for the patient; and has not the one become a rather nebulous proxy for the other?
About the Author:
At the time of writing this piece, Tim was the AMHP Lead for a central London local authority but he has recently retired from this role. He remains approved by his local authority and plans to do some sessional work as an AMHP from the autumn onwards.
Reference:
This piece makes regular reference to the following 2024 discussion paper by Matt Simpson, John Mitchell and Robert Lewis, entitled ‘MHA assessments’ and s13(1) MHA 1983: ‘New’ AMHP Practices within Existing Law:
Link to the full s13 (1) e-book: